Earlier May Be Better for Isolated Cleft Palate Surgery
Surgery at six months more likely to benefit a child's speech
In Brief:
- NIDCR-supported researchers conducted an international study on the timing of surgery for babies born with isolated cleft palate.
- The results suggest surgery at six months is more likely to benefit these children.
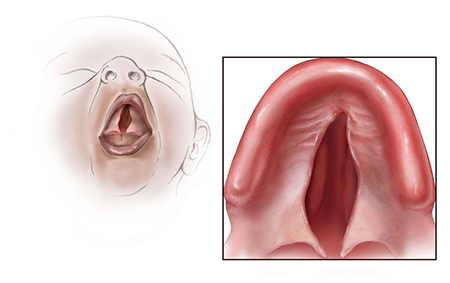
Every day around the globe, parents meet with doctors to discuss surgery to repair their newborn baby’s cleft palate, a congenital malformation of the roof of the mouth. An especially difficult part of this conversation involves weighing the pros and cons of operating at around six months or waiting for at least a year.
That’s because there’s no definitive study to consult, and the few that have been published are hard to compare because of their different designs and outcomes. While these studies suggest that surgery at six months can help put infants on track earlier to begin babbling and acquiring language like other children, surgery this early can be more technically challenging. It also requires that the infants receive anesthesia at a younger age, which carries risks.
Now, a large NIDCR-supported randomized clinical trial offers fresh data for parents and surgeons to consider for infants born with an isolated cleft palate, a subtype of the condition that occurs in the absence of other birth defects. It affects an estimated 1 to 25 newborns per 10,000 births worldwide. The study, published recently in the New England Journal of Medicine, found that children who were healthy enough to have their cleft palates surgically repaired at six months were less likely by age five to have difficulty producing speech sounds than those who had surgery at one year.
Like the other studies, the results come with limitations, all rooted in the inherent anatomical, surgical, and developmental complexity associated with repairing a cleft palate. But this study, called the Timing of Primary Surgery (TOPS) trial, establishes the feasibility of conducting a large, multinational randomized clinical trial and serves as a model for future efforts to generate comparable, high-quality data on speech outcomes.
Cleft palate is the most common facial birth defect, occurring alone or as part of a broader syndrome affecting other parts of the body. In both cases, the cleft appears in the embryo when the developing tissues that join to form the roof of the mouth, or palate, don’t fuse properly. An opening remains between the palate and nose that can make feeding difficult after birth. The cleft also can adversely affect the development of speech, hearing, dental health, and quality of life.
Though a first, or primary, corrective surgery during infancy, coupled with language therapy, can help to improve speech, about 30% of children still experience what’s called velopharyngeal insufficiency. It occurs when the soft palate fails to close tightly between the mouth and the nose during speech, causing air to escape from the nose and difficulties in producing specific speech sounds.
With so much still to learn about the timing of the surgery, an international collaboration of cleft specialists and researchers in Europe (Denmark, Norway, Sweden, and the United Kingdom) and in Brazil received NIDCR funding several years ago to conduct the TOPS trial. Leading the collaboration were William Shaw, B.D.S., D.Orth., Ph.D., University of Manchester, U.K.; and Carrol Gamble, Ph.D., University of Liverpool, U.K.
The U.K. researchers and their collaborators wanted to know: Does the timing of the corrective surgery truly influence a child’s development of speech? They also were interested in its influence on hearing and subsequent facial development.
To get an answer, the researchers enrolled 558 infants at 23 centers in Europe and South America.
Each infant was randomly assigned to undergo this initial surgery either at six or 12 months. For comparison purposes, all received the same standardized surgery to repair their cleft palate. It’s important to note that all centers specialized in oral surgery and care for babies born with a cleft palate.
The speech of all children was assessed at age five, an unprecedented length of follow-up for this type of study. During the follow-up, the researchers analyzed speech recordings for almost 84% of the six-month group and about 82% of the one-year group. It was no small feat.
“The analysis of the speech recordings required 41 speech and language therapists from participating sites to travel to the U.K. to assess the speech recordings at one-, three-, and five-year time points,” said Dr. Gamble. “This resulted in rich and complex data for analysis.”
Based on the evaluation of the recordings and other analyses, the TOPS researchers determined:
- Velopharyngeal insufficiency was less frequent in the six-month group (9%) than in the 12-month group (15%).
- Postoperative complications were infrequent for both groups.
- Hearing and middle ear function were poorer in the group about to have surgery at the year mark. However, these group differences weren’t detected at ages three and five, suggesting the hearing-related benefit of having the operation earlier doesn’t last over time.
- At five years, those in the six-month group were more likely to have dental arch constriction, meaning their opposing teeth weren’t positioned properly. It can cause a misaligned bite and affect the proportional growth of the midface. However, the differences in facial development between groups was not considered clinically meaningful at five years.
The researchers noted that their data are consistent with three of the four previously published studies on the timing issue. However, they also noted that their results don’t generalize to all forms of cleft palate.
For example, infants with a much more common form of cleft palate, called syndromic palate, were not included in the study. Neither were infants enrolled who were deemed medically unfit for surgery or had clefts that were considered too wide and more challenging to repair. The study also didn’t evaluate the influence of a second corrective surgery on children by age five.
“The TOPS study is a prime example of the accomplishments that are possible when several research disciplines pull together around a clinical problem,” said NIDCR Director Rena D’Souza, D.D.S., Ph.D. “There’s certainly much more to learn about the timing of surgery to repair an isolated cleft palate, but TOPS also shows that high-quality clinical research can help provide answers on this complex topic.”
Related Links:
Reference:
Gamble C, Persson C, Willadsen E, Albery L, Soegaard Andersen H, Zattoni Antoneli M, et al. Timing of Primary Surgery for Cleft Palate. N Engl J Med. 2023 Aug 31;389(9):795-807. doi: 10.1056/NEJMoa2215162.
Attention Editors
Reprint this article in your own publication or post to your website. NIDCR News articles are not copyrighted. Please acknowledge NIH's National Institute of Dental and Craniofacial Research as the source.
Subscribe for NIDCR Updates
Receive email updates about the latest advances in dental, oral, and craniofacial research.
November 2024