A Census Inside Your Mouth
Scientists characterize the mouth’s cells to gain insight into gum disease
In Brief:
- Scientists catalogued 120,000 oral mucosa cells by type and function, revealing a role for connective tissue cells in orchestrating immune responses linked to periodontitis.
- The cell atlas is designed to serve as a detailed community resource to help researchers answer key questions about oral biology and disease.
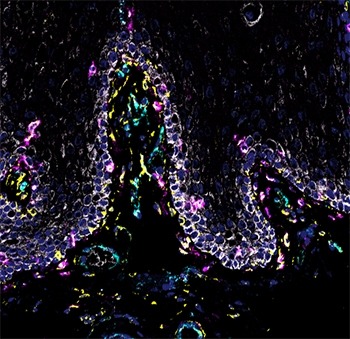
Eating, drinking, and breathing may seem simple and routine, but these daily acts constantly challenge the mouth. That’s because they expose our mouths to microbes and allergens from the outside world, and to micro-injuries from biting and chewing. Thanks to the oral mucosa—the protective mucous membrane that lines the inside of the mouth—the oral cavity is remarkably efficient at warding off pathogens and healing wounds, allowing us to live without the constant threat of infection and disease. Yet scientists don’t fully understand what makes the oral mucosa so resilient, or how it can become vulnerable to diseases like periodontitis (gum disease).
To help answer these questions, NIDCR researchers conducted a census of oral mucosal cells from gum and inner cheek tissues of people with and without severe periodontitis. By analyzing gene expression cell-by-cell, the scientists were able to catalog cells by type and function and reveal a previously unknown role for connective tissue cells in orchestrating immune responses linked to periodontitis. The results were published June 14 in the journal Cell.
“There’s been a huge international effort to create a cell-by-cell atlas of the human body,” says senior author Niki Moutsopoulos, DDS, PhD, a principal investigator at NIDCR. That initiative, called the Human Cell Atlas, was launched in 2016 and is led by scientists at the Broad Institute in Cambridge, Massachusetts, and the Wellcome Sanger Institute in Cambridge, UK. “We wanted to do our part by contributing data from the oral mucosa,” Moutsopoulos says.
Scientists have known that the oral mucosa is composed of four main types of cells. Epithelial cells form the surface layer of the oral mucosa, while endothelial cells line the blood vessels that supply nutrition and oxygen. Stromal cells give structure to the mucosa, and immune cells survey the surroundings to capture and destroy foreign particles.
However, Moutsopoulos’ team performed a deeper dive, identifying distinct subpopulations with unique traits and functions among the four cell types. One type of stromal cell—called fibroblasts—caught the research team’s eyes.
“The most striking part of the study was the prominent immune signature of fibroblasts in the oral environment,” says Moutsopoulos. “We usually think of stromal cells, such as fibroblasts, as mere producers of connective tissue, but our analyses suggest that they also play a role in immune function, particularly related to recruiting neutrophils.”
Neutrophils are immune cells that migrate into the oral cavity to defend us against pathogens and are thought to play a protective role against periodontitis. In fact, genetic deficiencies in neutrophil recruitment are linked to severe periodontitis. However, neutrophils are also known to over-congregate in the gums of people with common forms of periodontitis.
Gene expression data from the new study suggests that stromal cells are wired to induce inflammatory responses and send signals that recruit neutrophils in healthy people. The same stromal cells appear to become over-activated in periodontitis, resulting in an exaggerated immune response that could contribute to disease progression.
“This new piece of information is one of the many insights that can be gleaned from the oral cell catalog,” says first author Drake Williams, DDS, PhD, a clinical research fellow at NIDCR. “Another opportunity afforded by this atlas is that we were able to map the expression of genes linked to periodontitis susceptibility at the cell level, within the oral tissues. We envision that this information will provide clues towards understanding cell-specific functions that mediate periodontitis pathogenesis in different subsets of patients.”
The oral cell catalog can also be used to understand oral diseases beyond periodontitis. The data from healthy volunteers, who were carefully screened for oral and systemic health, serves as a baseline that can be compared against other disease states.
Moutsopoulos and her team have contributed their cell atlas to the oral and craniofacial network of the Human Cell Atlas project. They plan to expand the catalog to include cells from patients with inherited forms of oral mucosal diseases.
“The study provided an opportunity to view the oral mucosa through a new lens,” says Moutsopoulos. “We really enjoyed putting it together and had fantastic colleagues that contributed to this effort.”
Related Links
- Scientists Find Evidence that Novel Coronavirus Infects the Mouth’s Cells
- How Fungus Finds a Foothold in the Mouth
Reference
Human oral mucosa cell atlas reveals a stromal-neutrophil axis regulating tissue immunity.Williams DW, Greenwell-Wild T, Brenchley L, Dutzan N, Overmiller A, Sawaya AP, Webb S, Martin D; NIDCD/NIDCR Genomics and Computational Biology Core, Hajishengallis G, Divaris K, Morasso M, Haniffa M, Moutsopoulos NM. Cell. 2021 Jul 22;184(15):4090-4104.e15. doi: 10.1016/j.cell.2021.05.013. Epub 2021 Jun 14. PMID: 34129837.
NIH Support: In addition to NIDCR, support for this research came from the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
Attention Editors
Reprint this article in your own publication or post to your website. NIDCR News articles are not copyrighted. Please acknowledge NIH's National Institute of Dental and Craniofacial Research as the source.
Subscribe for NIDCR Updates
Receive email updates about the latest advances in dental, oral, and craniofacial research.
November 2024