Looking Forward to Greater IMPACT on Temporomandibular Disorders
Building a patient-centric research focus
In Brief:
- November is National TMJ Awareness Month. It highlights not only the significant impact temporomandibular disorders have in our society, but the research that continues to bring hope for improved care.
- NIDCR’s research efforts have helped to expand understanding of these disorders and orofacial pain in general.
Today, most treatments are designed for the “average patient.” But not everyone is an average patient. That’s true when treating people for cancer, diabetes, cognitive disorders, or even the common flu. That’s also especially true when caring for those with one of the temporomandibular disorders (TMDs). TMD is an umbrella term for more than 30 conditions that cause pain and dysfunction in the jaw joints and/or the muscles that control their movement. They affect 5% to 10% of the U.S. population and occur twice as often in women than men.
Did You Know?
November is National TMJ Awareness Month. Watch this video to learn how a healthy temporomandibular joint (TMJ) controls mouth opening and closing.
For more information on TMDs, including symptoms, diagnosis, treatment, and helpful tips, visit our temporomandibular disorders page. This information is also available in Spanish.
TMDs involve a complex interplay of biological, physiological, psychological, and environmental factors that have a range of possible symptoms, all of which affect people differently. For some, TMDs are painful but resolve relatively quickly with no lasting effects; for others, the disorder turns chronic and debilitating, affecting the ability to speak, eat, and even smile.
But complexity can be viewed as order waiting to be deciphered. For over six decades, NIDCR has supported basic, translational, and clinical research on TMDs and the mechanisms of pain to cut through this web of complexity. This growing base of knowledge will inform team efforts to tailor care to the individual needs of each patient. That includes using genetic, molecular, and clinical data to develop greater diagnostic precision, as well as factoring in preexisting conditions that may mask or modify the symptoms of TMD. It also includes treating the whole person and not assuming they are an average patient.
“For too many years, too many people with TMDs have not received care that is patient-centered largely because of the complexity of orofacial pain,” said NIDCR Director Rena D'Souza, D.D.S., Ph.D. “That must change. Through the power of innovation and collaboration, we can expand the evidence base, while also generating compelling new investigative leads. That’s something we can all look forward to during NIDCR’s 75th anniversary year and in the decades that lie ahead."
Making an IMPACT
One NIDCR-led effort to keep a hopeful eye on is the TMD Collaborative for IMproving PAtient-Centered Translational Research (TMD IMPACT). This collaborative, based in part on recommendations from a recent National Academy of Sciences, Engineering, and Medicine consensus study on TMDs, is intended to serve as a much-needed national research collaborative to accelerate progress on these disorders.
NIDCR recently issued nine TMD IMPACT planning grants totaling $2.8 million to research institutions across the country. The awardees are tasked to collectively design a gateway for researchers across the sciences to come together to conduct basic, translational, and clinical studies on these conditions. The aim is for these studies to fill known gaps with high-quality data to improve diagnosis, prevention, and treatment of TMDs.
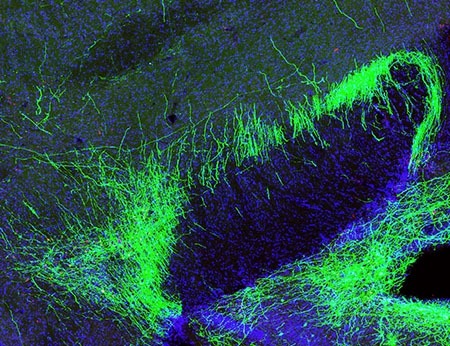
This collaborative, though intended to serve as a cornerstone of NIDCR’s current research on TMDs, is still just part of a broader institute and NIH investment in pain research. NIDCR’s portfolio includes studies now underway through NIH’s Helping to End Addiction Long-term® Initiative, or NIH HEAL Initiative®, which is actively exploring new non-addictive approaches to treat pain. A promising case in point is the recent discovery of a tract of pain-suppressing neurons in the brain that facilitate the numbing effects of general anesthesia. These NIDCR-supported findings could help scientists develop non-opioid medications that act on these neurons to treat chronic pain.
NIDCR participates in another HEAL effort called Restoring Joint Health and Function to Reduce Pain Consortium (RE-JOIN). Consortium scientists are systematically mapping out the network of sensory neurons that connect to two orthopedic joints: the jaw joints and the knee. They are particularly interested in how changes in these sensory neurons correlate with tissue degradation, inflammation, and pain. What’s learned will provide more possible targets to better control TMD pain.
NIDCR’s portfolio also enlists the innovative ideas of basic researchers from around the country. That includes those involved in an NIDCR effort to compare the gene activity inside individual cells extracted from healthy and diseased jaw joints. Toggling between the two can point to possible trouble spots in the diseased cells.
“Though this research is in its very early stages, it illustrates a great clinical need going forward: a way for clinicians to sample cells from a patient and look inside them to identify the drivers of a disease process,” said Jason Wan, Ph.D., director of NIDCR’s Mineralized Tissue Physiology Program.
The trouble spots will vary from person to person. Determining which ones have gone awry in each individual patient could help in accurately diagnosing the precise form, or subtype, of a disease that’s afflicting a patient. It also could guide them to the best available treatments for each patient and help to avoid spending time and money on those that won’t work.
Decades of Pain Research Progress
All of the above builds on NIDCR’s decades of achievement in pain research. That prominently includes pain of the face and mouth, called orofacial pain, of which TMDs are a leading cause. Orofacial pain affects an estimated 16% to 22% of U.S. adults, whether from injury, oral disease including cancer, or as a part of pain conditions that can manifest throughout the body.
During the latter half of the 20th century, institute scientists and grantees were instrumental in helping to define the anatomy, physiology, pharmacology, and genetics of pain. In the institute’s Neurobiology and Anesthesiology Branch, established in the early 1970s, researchers made many seminal discoveries. These include the identification of two distinct types of pain-sensing neurons in the brain stem’s trigeminal nerve system. This system relays pain signals from the face and mouth to the brain. These researchers also led pioneering studies to measure the electrical and chemical activity of neurons, track the travel routes of pain signals, understand how environmental information is processed in the nervous
system, more accurately measure the sensation of pain, and more effectively control pain during dental surgery. All this and a great deal of other work was guided by one philosophy: To study pain is to understand the brain.
During this time, research at NIDCR and elsewhere helped to establish that pain is more than a sensory phenomenon. It established that pain is an unwelcome sensation that each person is wired to interpret differently.
In fact, studies during this time found that long-lasting (chronic) pain can prompt changes throughout the body, affecting not only the central nervous system but the immune and hormonal systems. These systemic changes can transform chronic pain into a disease unto itself, not just a symptom linked to a clinically recognized disorder.
In the 21st century, NIDCR scientists and grantees continue to advance research on pain, and more broadly, somatosensation. This process encompasses our senses of touch, pain, temperature, and our bodies’ positions in space. These advances include the institute’s support of two co-recipients of the 2021 Nobel Prize in Physiology or Medicine:
- David Julius, University of California, San Francisco, who was recognized for his discovery of the first protein receptor controlling thermosensation, the body’s perception of temperature
- Ardem Patapoutian, Scripps Research Institute, La Jolla, California, who was honored for his seminal work that identified the first protein receptor that controls the sense of touch
Classic OPPERA
NIDCR also is proud to have supported the landmark Orofacial Pain: Prospective Evaluation and Risk Assessment (OPPERA) study. This large, national study enrolled 3,258 adults and followed them for nearly three years on average. The researchers identified a total of 202 risk factors that can underlie the development of acute TMD pain and its transition to a chronic pain condition. They also published more than 30 peer-reviewed journal articles detailing their findings. Those findings show that when TMDs persist in the jaw and advance to a chronic pain disorder, they often become part of a broader pain syndrome that involves other parts of the body and which, collectively, can change a person’s sense of well-being.
But OPPERA was an opening act, not a denouement. Today, other studies are picking up its clinical narrative to advance understanding of orofacial pain and its management. That includes an NIDCR-supported clinical trial called Understanding Laser Light Treatment Applications for TMD (ULLTRA-TMD). It will enroll approximately 100 people with TMD-related pain to evaluate low-level laser therapy, a treatment that has shown promise in controlling pain associated with other musculoskeletal conditions, possibly by decreasing inflammation.
While TMDs remain a web of challenging complexity for clinicians and basic scientists, NIDCR continues to invest in a better future for TMD care. In its 75th anniversary year, NIDCR looks forward to a future where not all patients are average, and more personalized care, grounded in scientific evidence, will be available for more people with TMDs and other orofacial pain disorders.
Related Links:
- Deconstructing TMJD Classifiers at the Single Cell Level
- NIDCR Funded Winners of 2021 Nobel Prize in Physiology or Medicine
- Inflammation May Curb, Not Cause, Chronic Pain
- How Sound Reduces Pain in Mice
- Facial Pain Comes to Light
- Dialing Down Pain from the Brain
- Converging Pathways of Pain Research at NIDCR
Attention Editors
Reprint this article in your own publication or post to your website. NIDCR News articles are not copyrighted. Please acknowledge NIH's National Institute of Dental and Craniofacial Research as the source.
Subscribe for NIDCR Updates
Receive email updates about the latest advances in dental, oral, and craniofacial research.
November 2024