Facing Cancer Head-On
Did You Know?
April is Oral Cancer Awareness Month. NIDCR offers resources for the general public to raise awareness of oral cancer:
- For easy-to-read information on oral cancer and other dental, oral, and craniofacial conditions, visit our Health Info page. This information is also available in Spanish.
Watch a video where NIDCR clinicians show you what to expect during an oral cancer exam. An exam allows health care providers to detect early signs of cancer in the mouth.
This year, an estimated 65,000 people in the United States will be diagnosed with head and neck cancers. This group of diseases includes cancers of the larynx (voice box), throat, lips, oral cavity, nose, and salivary glands. While prevention measures such as tobacco control and smoking cessation have reduced head and neck cancers overall, oral cancer associated with human papillomavirus (HPV) infection has steadily increased in recent years. Because head and neck cancers often go undetected until they’re quite advanced and are difficult to treat, the survival rate remains around 40-50%, and cancer is likely to recur after treatment.
Patients often experience diminished quality of life. “Many patients with head and neck cancer experience pain, either from the tumor or from treatments like surgery and radiation,” said oncologist Barbara Burtness, M.D., of Yale University. “Even for patients who have been cured, the treatments can result in difficulty swallowing, depriving people of the pleasure of eating and social connection from dining together. Some patients also report chronic pain, speech impairment, or hearing loss.”
To improve patient outcomes, NIDCR-supported researchers have been tackling head and neck cancers from multiple angles. In addition to traditional chemotherapy and radiation therapy, many scientists are tapping into immunotherapy, leveraging the immune system with cancer vaccines and tumor-killing therapies. Others are investigating the crosstalk between cancer cells and nerves that promotes disease progression. In the clinic, scientists are developing devices and computer algorithms to help dental professionals map suspicious lesions in the mouth for biopsies and early detection. Researchers are also studying HPV vaccine implementation, hesitancy, and uptake. In many cases, these research efforts have been supported through partnerships with the National Cancer Institute (NCI), including the recently launched Advancing Head and Neck Cancer Early Detection Research (AHEAD) initiative.
“While we have gained a wealth of knowledge about the biology of head and neck cancers over the past decades, the statistics around their morbidity and mortality show there is much more work to be done,” said NIDCR Deputy Director Jennifer Webster-Cyriaque, D.D.S., Ph.D. “These discoveries must be translated into practical solutions — prevention strategies, early detection methods, and novel therapies — for the benefit of all patients.”
The Network that Feeds Cancer
Clinicians have had limited success in tackling cancer partly because the disease has a strong support system. The networks of connective tissue, blood vessels, and nerves that surround tumor cells mutually support each other in a way that fuels cancer development and progression.
A recent study at MD Anderson Cancer Center showed that mice lacking p53, a protein that normally restrains cancer growth, had denser nerve networks around oral tumors than mice with p53. First author Moran Amit, M.D., Ph.D., senior investigator Jeffrey Myers, M.D., Ph.D., and their colleagues found that the loss of p53 allowed tumor cells to reprogram healthy nerves into cancer-promoting ones. They confirmed the finding in oral cancer patients and revealed that p53 status was associated with nerve density and poor clinical outcomes. The research suggests that interrupting crosstalk between tumors and nerves may lead to potential therapies.
Nisha D’Silva, B.D.S., M.S.D., Ph.D., and her team at the University of Michigan devised a metric to further articulate the tumor-nerve relationship by measuring nerve density around tumors. The group found that higher nerve density enhanced tumor growth in animals and was associated with lower oral cancer survival rates in humans. The method could one day help clinicians identify aggressive tumors and inform the best course of treatment.
Tapping into the Body’s Defense System
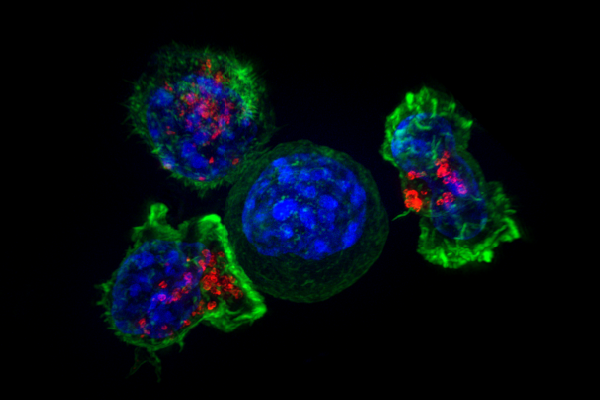
Cancers are cunning. To avoid attacks from the immune system, cancer cells can display proteins on their surfaces that disguise them as healthy cells. Clinicians have been prescribing a type of immunotherapy called immune checkpoint inhibitors, which counteract these protein disguises to enable the immune system to recognize and kill tumor cells. This class of drugs has shown promise for treating a small percentage head and neck cancers, as well as other types of cancers, such as lung and skin cancers.
Unfortunately, many cases of head and neck cancer are resistant to these therapies — only 15-20% of patients respond to them. Dr. Burtness, the Yale oncologist, wants to fix that. Her team is funded by NIDCR and NCI through the Specialized Programs of Research Excellence (SPORE), an NCI initiative to rapidly move basic science findings into clinical interventions. The Yale scientists plan to identify cancer-driving biological pathways unique to head and neck cancer to develop more effective therapies. They're exploring treatments that trigger deadly DNA changes in cancer cells in combination with immune checkpoint inhibitors, and they aim to verify their findings in clinical trials.
At the Dana-Farber Brigham Cancer Center, head and neck cancer surgeon Ravindra Uppaluri, M.D., Ph.D., is investigating another strategy: cancer vaccines. Like traditional vaccines that train the immune system to recognize and kill viruses, cancer vaccines teach the body’s immune cells to recognize cancer-specific proteins on tumor cell surfaces. Using a mouse model of head and neck cancer, Dr. Uppaluri’s group asked why certain vaccines generate strong responses while others do not.
They tested two different vaccines that act against tumor cell proteins called mICAM1 and p15E. Both vaccines triggered a response from cancer-killing immune assassins called CD8+ T cells. However, the mICAM1 vaccine additionally elicited a reaction from CD4+ T cells, which help enhance immune attacks. Compared to mice given the p15E vaccine, mICAM1-vaccinated mice had slower tumor growth and survived longer, highlighting a role for CD4+ T cells in boosting immune responses to cancer. The findings may help researchers understand how to develop better head and neck cancer vaccines.
Dr. Uppaluri also received a Cancer Moonshot grant co-funded by NCI and NIDCR through the Immuno-Oncology Translational Network. Cancer Moonshot is a White House initiative led by NCI to accelerate cancer research, improve patient care, and end cancer as we know it. Network scientists aim to improve immunotherapy outcomes and prevent cancers before they occur. Dr. Uppaluri is working to understand the biology of immunotherapy resistance in head and neck cancers.
In a clinical trial, Dr. Uppaluri and his team treated patients with two doses of a type of immune checkpoint inhibitor called anti-programmed cell death protein 1 before surgically removing head and neck tumors. They found that 45% of the patients had some response to this treatment, including signs of cancer cell death in the collected tumors under the microscope. They also discovered that people who responded well to the treatment had higher levels of certain immune cells compared to those whose tumors were resistant. The findings suggest that the activation of these immune cells is crucial for successful therapy and could help clinicians identify patients who may respond better to these therapies.
Nipping Head and Neck Cancer in the Bud
Another facet of NIDCR’s head and neck cancer research focuses on finding ways to lower the risk of cancer developing in the first place. Scientists have identified certain risk factors for head and neck cancers, including HPV infection, heavy alcohol use, and cigarette smoking. Studies have shown that reduced cigarette smoking in recent years is linked to declining rates of tobacco-associated head and neck cancer. But growing evidence also suggests that e-cigarette use, or vaping, may be just as harmful as cigarette smoking.
A team led by Ahmad Besaratinia, Ph.D., M.P.H., at the University of Southern California found that vapers and smokers had similar levels of DNA damage in oral cavity-lining cells — more than twice the amount found in non-users. DNA damage is early changes in cells that can contribute to cancer and other chronic diseases. In the study, the more a person smoked or vaped, the more DNA damage there was, suggesting that vaping may be just as likely as cigarette smoking to cause changes potentially relevant to cancer in the mouth.
Catching cancer early and intervening promptly can change the course of disease progression. When head and neck cancer is detected early, patients have a five-year survival rate of up to 80%, compared to about 20% for late-stage disease. The gold standard for screening is to biopsy suspicious tissues, a technique that relies heavily on the experience of the clinician. Knowing when and where to look can be challenging, even for the most seasoned providers.
Scientists at Rice University and MD Anderson Cancer Center, led by Rebecca Richards-Kortum, Ph.D., designed a portable imaging system to help clinicians spot suspicious oral lesions. This system can create a cancer risk and biopsy guidance map based on photos, fluorescence imaging, and microscopy images of the patient’s oral tissues. These maps are then physically projected onto the patient’s mouth, highlighting the most suspicious-looking areas where clinicians should consider taking biopsies. This real-time visualization process can be completed by clinicians in just minutes. The research team is working to further optimize the system to enhance its diagnostic potential.
Most recently, NIDCR partnered with NCI to launch the AHEAD program, which aims to promote biomarker development to help clinicians detect cancer early, prevent cancer growth, and monitor treatment responses to curb recurrence. Biomarkers are molecules found in blood, body fluids including saliva, or tissues that predict or signal the presence of cancer. In 2023, NIDCR, together with NCI, awarded seven grants totaling $4.4 million for up to five years of support. With access to NIDCR and NCI resources and infrastructure, such as NCI’s Early Detection Network, researchers are mapping the immune, genetic, and protein changes that drive suspicious oral lesions into cancers.
“NIDCR-supported research has patients’ best interests in mind,” said Zhong Chen, M.D., Ph.D., director of NIDCR’s Oral and Salivary Cancer Biology Program. “We are in a very exciting era with fascinating technological advances in biology, medicine, and computation that will move us collaboratively toward a future where head and neck cancer can be better prevented, diagnosed earlier, and treated more effectively.”
Related Links:
References:
- Amit M, Takahashi H, Dragomir MP, Lindemann A, Gleber-Netto FO, Pickering CR, et al. Loss of p53 drives neuron reprogramming in head and neck cancer. Nature. 2020 Feb;578(7795):449-454. doi: 10.1038/s41586-020-1996-3. Epub 2020 Feb 12.
- Perez-Pacheco C, Schmitd LB, Furgal A, Bellile EL, Liu M, Fattah A, et al. Increased Nerve Density Adversely Affects Outcome in Oral Cancer. Clin Cancer Res. 2023 Jul 5;29(13):2501-2512. doi: 10.1158/1078-0432.CCR-22-3496.
- Shibata H, Xu N, Saito S, Zhou L, Ozgenc I, Webb J, et al. Integrating CD4+ T cell help for therapeutic cancer vaccination in a preclinical head and neck cancer model. Oncoimmunology. 2021 Aug 10;10(1):1958589. doi: 10.1080/2162402X.2021.1958589.
- Oliveira G, Egloff AM, Afeyan AB, Wolff JO, Zeng Z, Chernock RD, et al. Preexisting tumor-resident T cells with cytotoxic potential associate with response to neoadjuvant anti-PD-1 in head and neck cancer. Sci Immunol. 2023 Sep 8;8(87):eadf4968. doi: 10.1126/sciimmunol.adf4968.
- Tommasi S, Blumenfeld H, Besaratinia A. Vaping Dose, Device Type, and E-Liquid Flavor are Determinants of DNA Damage in Electronic Cigarette Users. Nicotine Tob Res. 2023 May 22;25(6):1145-1154. doi: 10.1093/ntr/ntad003.
- Coole JB, Brenes D, Mitbander R, Vohra I, Hou H, Kortum A, et al. Multimodal optical imaging with real-time projection of cancer risk and biopsy guidance maps for early oral cancer diagnosis and treatment. J Biomed Opt. 2023 Jan;28(1):016002. doi: 10.1117/1.JBO.28.1.016002. Epub 2023 Jan 13.
Attention Editors
Reprint this article in your own publication or post to your website. NIDCR News articles are not copyrighted. Please acknowledge NIH's National Institute of Dental and Craniofacial Research as the source.
Subscribe for NIDCR Updates
Receive email updates about the latest advances in dental, oral, and craniofacial research.
October 2024