Oral Health in America - May 2022 Bulletin
Section 3B Summary
Oral Health Across the Lifespan: Older Adults
The U.S. population 65 years of age and older is growing rapidly. Today, 1 in 6 Americans is over the age of 65, and by 2030 that proportion will increase to 1 in 5. The older adult population will be one of the most diverse ever in terms of race/ethnicity, socioeconomic status, health, and functional status. With an aging population and increased expectations for good oral health-related quality of life, more older Americans are seeking dental care. Complicating matters, many adults lose their private dental insurance when they retire, leaving them with little to no coverage during a stage of life where their need for oral healthcare may be greater than ever.
Status of Knowledge, Practice, and Perspectives
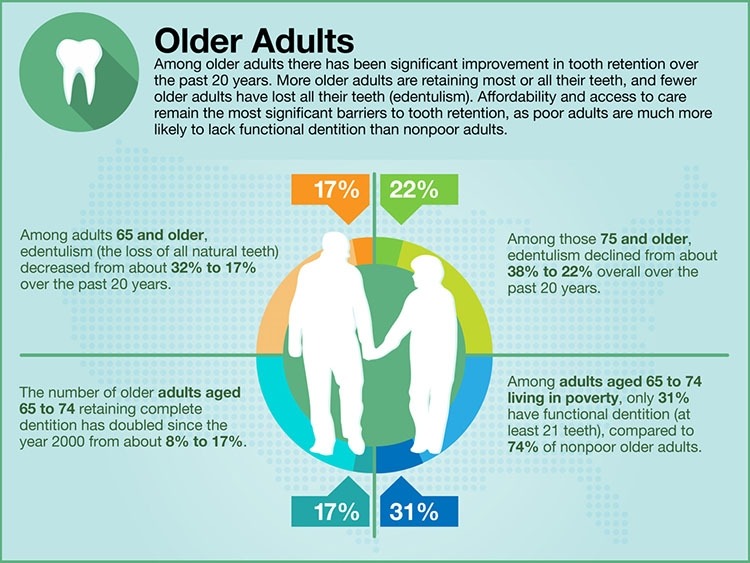
About 80% of older Americans live with a chronic disease and nearly 70% have at least two chronic diseases. As these diseases progress, physical and neurobiological changes become more likely and can lead to disabilities that affect an individual’s capacity to maintain good oral self-care. Among adults over the age of 75, 54% have fewer than 21 remaining teeth and the proportion increases to 80% for those living in poverty. With age comes the increased prevalence of systemic diseases that may impact the mouth, making older adults more susceptible to oral health issues.
Advances and Challenges
While tooth loss remains a problem for older adults, the overall oral health of Americans over 65 has improved significantly over the past two decades. Older Americans are having fewer teeth extracted and the proportion of the population with edentulism (no remaining teeth) is at an all-time low. Greater attention to prevention and improvements in treatments for gum disease and dental caries, along with a decline in the rate of smoking, have contributed to more older adults keeping their teeth than any previous generation.
The most important challenge is the increasing cost of dental care. As more older adults retain their natural teeth or receive dental implants, access to ongoing preventive and restorative oral care becomes important for this age group. Accessing care is especially difficult for homebound adults; a 2013 study showed that 96% of the participants had not seen a dentist since they became homebound. New oral health guidelines and expansion of the oral health workforce that is trained to manage the care of older adults are needed to expand access to care for this vulnerable population.
Promising New Directions
Although further research is needed to establish its long-term effectiveness for the elderly, silver diamine fluoride is seeing a resurgence as a noninvasive treatment for root caries, and it has been shown to be effective, affordable, and safe for use in older adults. This treatment seems especially useful for homebound or institutionalized older adults because of its ease of application and minimal support equipment needed to deliver it. Additionally, increasing emphasis on interprofessional care and training can maximize the effectiveness of non-oral health professionals in oral health roles. Understanding the relationships between severe periodontitis and noncommunicable diseases, how to assess the health of periodontal tissues, and how to make a referral to a dentist can promote effective interprofessional care and improved general health.
Additional Takeaways
The older adult population is on course to outnumber the younger population (those under 18) by 2034. By 2060 nearly 1 in 4 Americans will be older than 65. This burgeoning population of older adults will increase the pressure on our oral healthcare system, which already has unequal distribution of services and costs that are prohibitive to many. The goal should be to ensure that older adults receive appropriate oral health care so the primary focus can be on maintenance and prevention rather than the complex restorative procedures that often become necessary after years of neglect.
Q&A with Section Editor
Q&A with Jocelyne Feine, DDS, MS, HDR, senior editor, Section 3B: Oral Health Across the Lifespan: Older Adults.
What are some important takeaways about this section?
The older population is rapidly increasing. By 2030, 20% of the population will be over the age of 65. Upon retirement, many older adults who could previously afford oral health care find themselves on fixed incomes and lacking insurance coverage. At the same time, their previous dental restorations begin to break down and require repair and/or replacement, which is costly and often unaffordable.
Older adults who have become either physically or cognitively disabled and are homebound/ institutionalized may no longer be able to maintain their own oral hygiene. Since daily oral hygiene is rarely provided by care givers and institutional staff, these disabled adults display high levels of oral bacteria that can result in rampant caries as well as cardiovascular and respiratory problems, including infective endocarditis and aspiration pneumonia.
Additionally, many older adults suffer from one or more chronic conditions for which they take medications. Many of these health conditions and medications cause xerostomia (dry mouth) which diminishes oral function and creates an environment that promotes caries and may cause taste alterations, oral ulcerations, and pain.
What was a surprising finding?
The lack of attention over the years to maintaining the oral health of older adults was surprising. Nursing home staff are untrained in cleaning mouths/teeth and this is typically not one of their listed duties. Although more older adults today have retained their teeth, their access to necessary oral health care and maintenance services remains unattainable to many.
What should the American people know about this section of the report?
Older Americans struggle to maintain their oral health for a variety of reasons, particularly because of the cost of dental care. Institutionalized and homebound older adults are particularly vulnerable to oral disease, since they often cannot independently maintain their oral hygiene. Chronic inflammatory conditions that are common to older Americans, such as cardiovascular disease and diabetes, are also associated with inflammatory dental diseases, such as periodontitis.
What is the main call to action?
Policy changes are needed to mandate provision of oral health care for older adults through Medicare. We should also provide dental students with education on aging and providing home/institutional visits to serve patients who are unable travel to the dental office due to physical/mental health issues.
Jocelyne Feine, DDS, MS, HDR, is a professor in the faculty of Dental Medicine and Oral Health Sciences at McGill University, Canada. She received her dental and master’s degrees from the University of Texas at Houston and was awarded the Habilitation à deriger des recherches (HDR) degree from the Universite d’Auvergne, France. Her research emphasizes chronic orofacial conditions, pain, tooth loss, and patients’ quality of life.
Did You Know?
Learn more about Oral Health in America: Advances and Challenges
July 2024