Oral Health in America - July 2022 Bulletin
Section 4 Summary
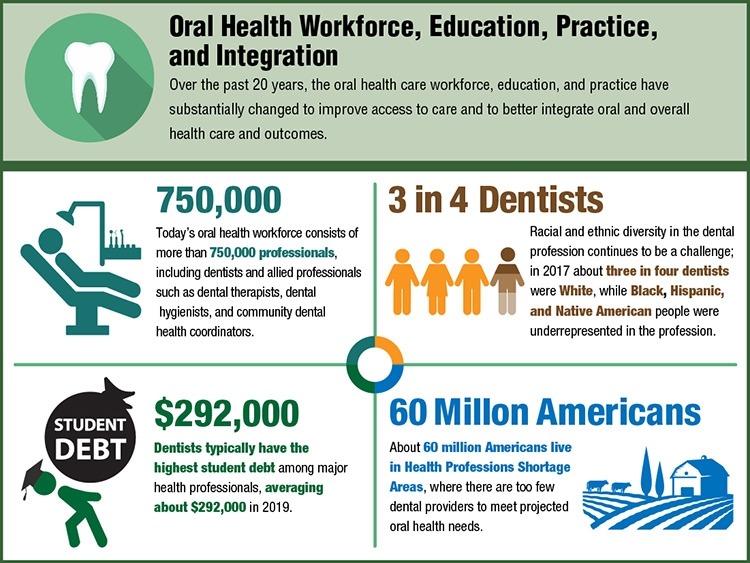
Oral Health Workforce, Education, Practice, and Integration
The oral health care system, including its workforce, education, practice, and financing, have transformed over the past 20 years to improve access to care for people who are underserved, enhance patient safety, and better integrate oral and general health care delivery. However, opportunities for further improvement remain. The oral health needs of the public, patients’ oral health literacy and behaviors, and policies shape the composition of the workforce, where new positions in dental practices and advanced training for clinicians are being developed. Practitioners can advance the accessibility and quality of the nation’s oral health by working with their colleagues in medical and behavioral systems of care, academia, insurance companies, and government agencies.
Status of Knowledge, Practice, and Perspectives
In 2020, the US oral health workforce consisted of more than 750,000 practitioners, including dentists, allied professionals such as dental hygienists, dental assistants, and dental laboratory technicians, as well as newer types of providers including dental therapists and community dental health coordinators. Private practices deliver most of the nation’s oral health care. With federal support for oral health infrastructure and service expansion of Federally Qualified Health Centers (FQHC), a growing number of people—nearly 5.2 million in 2020, up from about 1.4 million in 2001—have accessed oral health care services.
Advances and Challenges
Accessing oral health care can be difficult for people who are homebound due to age or disabilities and for those without access to transportation or with inflexible work hours. About 60 million Americans live in areas with too few providers to meet projected oral health needs. Some communities address these barriers by expanding dental hygienists’ roles and introducing dental therapists, who can provide preventative care and basic restorative procedures that have been traditionally carried out by dentists.
Racial and ethnic diversity in the dental profession remains a challenge. In 2017, nearly three out of four dentists were white, with disproportionate representation of Black, Hispanic, and Native American dentists. Dental education loan repayment and scholarship programs are essential tools for enhancing workforce diversity. With the high cost of dental education, dentists typically have the highest debt among health professionals; on average, dentists who graduated in 2019 had about $292,000 in student debt. High levels of debt may drive dentists to practice in affluent areas.
Promising New Directions
Co-location of dental and medical professionals, use of telehealth services, and provision of head and neck cancer or blood pressure screening by dental personnel can enhance access to and quality of oral health care. In addition, the scope of dental practice could potentially expand to include the monitoring of other chronic illnesses and vaccine delivery. Developing electronic dental records and integrating them with medical records can enable health professionals to provide coordinated services, measure oral health outcomes, and evaluate effectiveness of care. Community dental health coordinators can provide culturally sensitive health information, help people navigate health care services, and connect them with dental service providers.
Additional Takeaways
Changes are happening in dental education to address dental workforce diversity, including efforts to recruit a student population that reflects the diversity of the nation. Modifications in curriculum have also resulted in better integration of behavioral, clinical, and basic sciences, while students are being trained to provide comprehensive care and treat underserved patients in community-based settings.
Today, more people have dental insurance than 20 years ago, yet accessibility and the cost of dental care is out of reach for many. People with insurance are more likely to access dental services within a given year than those without. However, more than half of dentists do not accept public insurance, posing a challenge for Medicaid and Children’s Health Insurance Program recipients. Improving Americans’ access to oral health care requires coordinated efforts among policymakers, insurers, and dental professionals.
Q&A with Section Editor
Q&A with Kathryn Atchison, DDS, MPH, senior editor, Section 4: Oral Health Workforce, Education, Practice, and Integration.
What are some important takeaways about this section?
Dental therapists and community dental health coordinators are newer types of dental professionals who work in rural and urban areas to connect people who are underserved, including Native Americans, with dental care providers. A growing business model called Dental Service Organizations provides administrative support to dentists, enabling them to focus on providing dental care. Despite the large increase in the number of Americans with dental insurance since 2000, the current oral health care system does not meet the needs of all Americans.
What was a surprising finding?
I was surprised by the variety of population groups who report being unable to fully access the US oral health care system. Money is a necessity to obtain care, and having insurance seems like an excellent remedy, but many dentists do not accept public insurance. People in the LGBTQ+ community reported difficulties in getting appointments despite anti-discrimination laws. Adults with special health care needs find few dentists who can accommodate them. Many practices are usually open only on weekdays during business hours, which challenges people whose work does not offer flexible hours or medical release time.
What should the American people know about this section of the report?
Not all people can access private or public dental care, such as those who are homebound, institutionalized, have set work hours, or lack transportation to the dental office. We need to expand our offerings of non-traditional dental locations, including settings where children learn, where people live, and even where individuals shop or work so that everyone has access to dental care. These locations include day care centers, schools, assisted living centers, group homes for persons with disabilities, nursing homes, and rural community centers. Integrated managed-care organizations have also explored the value that interprofessional practice can add to patients’ overall health. Moreover, pediatricians have embraced providing oral health examinations, fluoride varnish, and oral health education to young children without dental coverage.
What is the main call to action?
The main call to action is to recognize that oral health care is an essential health care need of all Americans. Therefore, policymakers and oral health system stakeholders must work together to support an oral health care workforce and delivery system that provides oral health services as part of an integrated approach that will facilitate better oral and general health.
Kathryn Atchison, DDS, MPH, is a professor at the University of California, Los Angeles. She received a DDS from Marquette University and a Master of Public Health from Boston University. She is a dental educator with 20 years of experience in public health as well as clinical and health services research.
Did You Know?
Learn more about Oral Health in America: Advances and Challenges
July 2024