Our Jaw Shape May Foretell Risk of Temporomandibular Disorders
AI tool showed a smaller jawbone may increase risk
In Brief:
- An NIDCR-supported study showed that a smaller lower jawbone may strain the jaw joint and could predict a person’s risk of painful jaw problems.
- The findings may help explain why women and people with a certain form of overbite, who typically have smaller jaws, are more likely to develop temporomandibular disorders (TMDs).
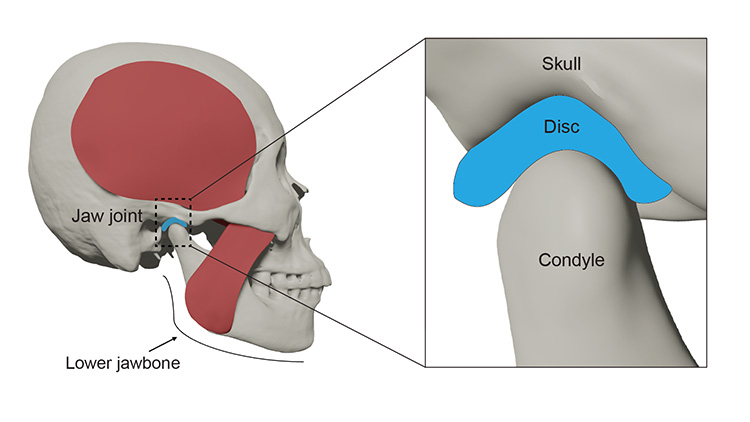
Pain and clicking in the jaw, tenderness in the chewing muscles, and recurring headaches can all be signs of jaw problems called temporomandibular disorders (TMDs). TMDs are a group of more than 30 conditions that can cause pain and dysfunction in the jaw joints, chewing muscles, and nearby tissues.
TMDs affect 5% to 10% of the U.S. population and occur twice as often in women than men. Studies show that a complex interplay of biological, psychological, and social factors drive TMDs, but how exactly remains unclear. Symptoms can often appear suddenly and vary widely among patients. Without a clear understanding of the underlying causes, it’s hard for clinicians to diagnose and treat TMDs effectively.
Now, aided by artificial intelligence (AI), scientists show that the shape of the jawbone itself might affect a person’s likelihood of developing a TMD. The NIDCR-funded study, published in JCI Insight, may help explain why TMDs are more common in women and people with certain forms of overbite.
The team set out to compare 3D scans of jawbones from people with and without TMDs. They were looking for structural differences that could help distinguish people with TMDs from people without them. Initially, the scientists attempted the task manually, comparing the images one by one.
"But our brains and eyes have limitations," said first author Shuchun Sun, Ph.D., of Clemson University and the Medical University of South Carolina. "We cannot see complex patterns in a lot of the 3D geometry on a computer screen, so why not use AI to help?"
The team developed an AI tool that scanned 3D jaw images from 40 people with TMDs and 40 without. It identified three areas of the lower jawbone that were shaped differently in people with TMDs.
Most notably, patients with TMDs had overall smaller lower jawbones. They also had smaller and flatter condyles, the rounded ends of the lower jawbone that fit into a cup-like hollow in the lower skull to form the joint.
The team then developed computer programs to simulate how these differences might affect how the jaw moves and functions. They used head scans from eight men and eight women who had passed away and did not have TMDs. The computer program predicted that people with smaller lower jawbones would need to put more force on the joint to achieve the same bite strength as people with larger jaws.
"A flat condyle has less surface area to distribute the force evenly, so simple tasks like chewing can strain the joint," said senior author Hai Yao, Ph.D., of Clemson University and the Medical University of South Carolina.
The computer program also predicted that people with smaller jaws may have less oxygen and nutrients available for energy production in the cartilage of the jaw joint. They may also be more likely to have higher levels of molecules associated with muscle fatigue. The results offer an explanation as to why women and people with certain forms of overbite — both of whom tend to have smaller jaws — may be more likely to develop TMDs.
These findings give researchers a starting point from which to explore whether the same mechanisms are at play in animals and humans. With more research, the scientists also hope that the AI tool may one day aid clinicians’ ability to diagnose TMDs and offer insights into treatment.
The team would like to use the same method to investigate other contributors to TMDs. These include features of the chewing muscles, inflammation levels, psychological stress, and pain perception. The method could also be useful for understanding other complex muscle and skeletal problems in the knee and spine.
“TMDs are very complex. It’s very difficult to predict the disease progression and how patients respond to treatments,” said Dr. Yao. “Patients need better diagnosis and personalized treatment, and AI is a powerful tool that can help us.”
Related Links
- Looking Forward to Greater IMPACT on Temporomandibular Disorders
- How Data Science and Digital Dentistry Can Improve Dental Care
Reference
Sun S, Xu P, Buchweitz N, Hill CN, Ahmadi F, Wilson MB, et al. Explainable deep learning and biomechanical modeling for TMJ disorder morphological risk factors. JCI Insight. 2024 Jul 11;9(16):e178578. doi: 10.1172/jci.insight.178578.
Attention Editors
Reprint this article in your own publication or post to your website. NIDCR News articles are not copyrighted. Please acknowledge NIH's National Institute of Dental and Craniofacial Research as the source.
Subscribe for NIDCR Updates
Receive email updates about the latest advances in dental, oral, and craniofacial research.
November 2024