Healthy Mouth, Healthy Body
Decades of NIDCR-funded research reveal the interconnectedness of the mouth and body
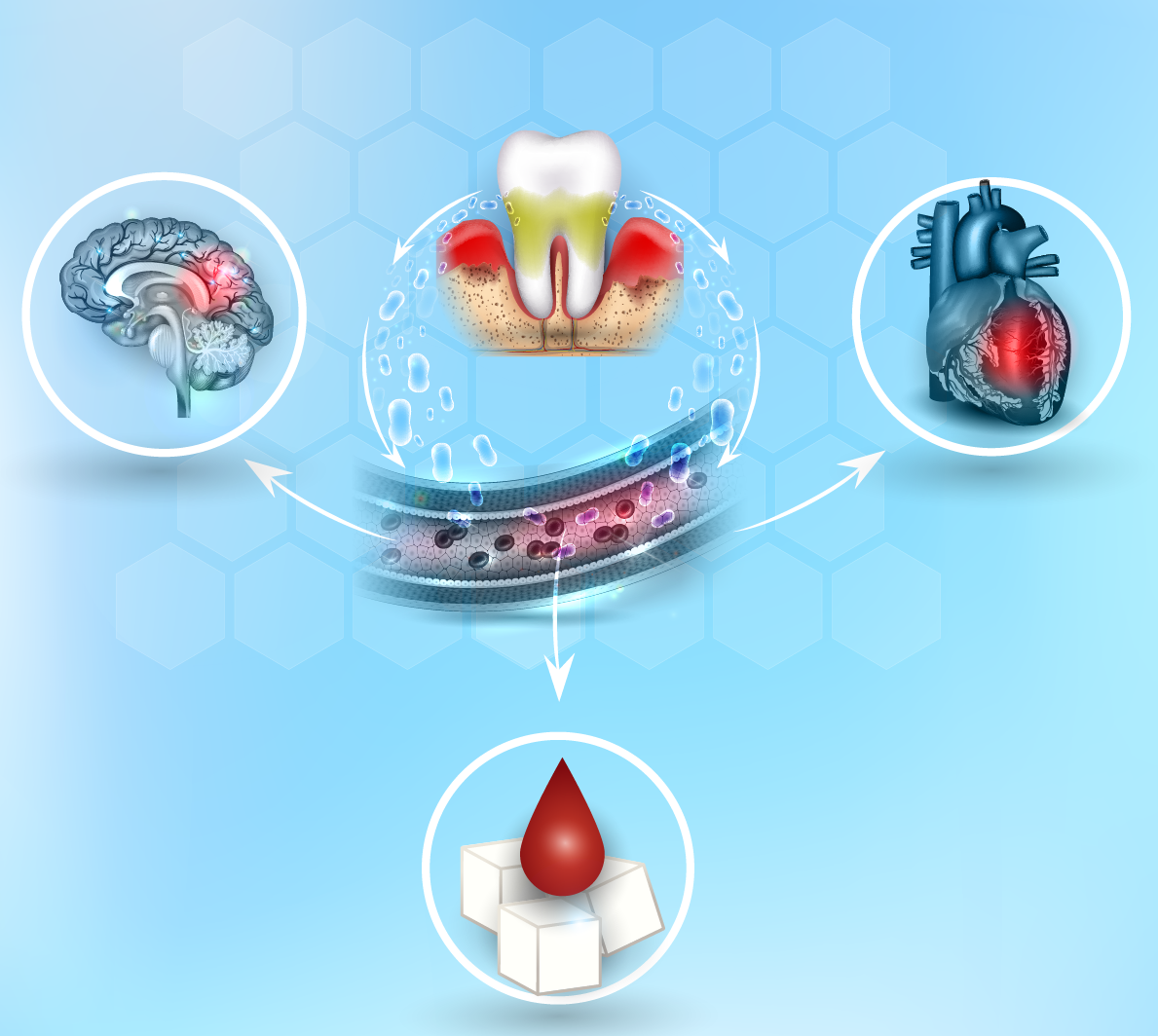
For the last 40 years or so, NIDCR has supported research on the biological links between the mouth and the rest of the body, commonly known as the "oral-systemic connection." In that time, scientists have unveiled a multitude of connections between oral diseases such as periodontal (gum) disease and tooth decay, and conditions like diabetes, dementia, cardiovascular (heart and vascular) disease, preterm birth, HIV, and even cancer. These connections suggest that having an oral disease could increase the risk of developing or worsening a systemic condition, and vice versa.
While the existence of these oral-systemic associations is well established, their exact causes are not clear. In some cases, scientists have found periodontal disease-causing bacteria in the diseased region of the body, suggesting these bacteria colonize other parts of the body and trigger illness beyond the mouth. In other cases, there is evidence that the characteristic inflammation of periodontal (gum) disease, driven by the body’s immune response to an overgrowth of pathogenic bacteria in the gums, can worsen inflammation in other parts of the body, which in turn may contribute to certain diseases. On the other hand, inflammation arising from conditions like heart disease and diabetes may worsen periodontal disease.
Periodontal disease and chronic systemic conditions like heart disease, stroke, and diabetes share risk factors such as smoking, poor diet, obesity, high blood pressure, or high LDL, or “bad” cholesterol. So, having one or more of these risk factors may make a person more likely to have both oral and systemic diseases.
More directly, the mouth is the physical opening into the digestive and respiratory tracts. Thus, when disease-related microbes are breathed in or swallowed, infections, ulcers, pneumonia, and possibly even cancer may result.
“Both dentists and physicians can benefit from being more familiar with the oral manifestations of systemic disease, allowing for earlier diagnoses and improved management of diseases to better help patients,” said NIDCR Deputy Director Jennifer Webster-Cyriaque, D.D.S., Ph.D. “Increased collaboration through continuing education and intentional communication between medical and dental providers can improve patient outcomes and maximize the public health benefit.”
For four decades, NIDCR-supported scientists have been working to decipher the relationships between the mouth and the rest of the body. What they’re finding may bring new insights into the interconnectedness of various systems in the body, as well as better treatments for both oral and systemic diseases.
What’s the Connection?
Diabetes
In the 1980s, some of the earliest modern research on the oral-systemic connection established a link between diabetes and periodontal disease. One study by State University of New York Buffalo scientist Robert Genco, D.D.S., Ph.D., found that people with diabetes were 15 times more likely to have lost all their teeth than those who didn’t have diabetes. The research, funded by the National Institute of Dental Research, or NIDR, as the institute was called until 1998, led Dr. Genco to claim that periodontal disease was among the top six health complications potentially resulting from uncontrolled diabetes.
Researchers theorize that high blood sugar in people with uncontrolled diabetes could promote the overgrowth of periodontal disease-causing bacteria in the mouth. However, randomized clinical trials aimed at establishing a direct connection between periodontal disease and diabetes — that is, studies testing whether treating one helps the other — have so far yielded inconclusive results. While periodontal disease treatment has shown to be beneficial for managing blood sugar levels in periodontitis patients at high risk of diabetes, high-quality randomized controlled trials are necessary to confirm these findings. Such trials are the gold standard for establishing a cause-and-effect relationship between oral and systemic health conditions. NIDCR funds ongoing research comparing the mouth’s microbiome before and after diabetes treatment to better understand the relationship between periodontal disease and diabetes.
Pregnancy Complications
In the 1990s, NIDR-funded researchers Steve Offenbacher, D.D.S., Ph.D., and James Beck, Ph.D., at the University of North Carolina (UNC) at Chapel Hill, found an association between periodontal disease in pregnant mothers and the risk of giving birth early and having babies with low birth weights.
The team later added high blood pressure in pregnancy, the potentially dangerous condition called preeclampsia, to the list of pregnancy complications linked to periodontal disease. Other investigators showed that the kinds of bacteria implicated in periodontal disease can end up in the human placenta. While these bacteria have been detected in the blood, how they travel to the placenta isn’t quite known yet. But like with diabetes, conclusive evidence that treating periodontal disease can improve or prevent pregnancy complications hasn’t yet emerged. To advance this line of investigation, NIDCR currently supports five research projects that aim to understand how maternal health during pregnancy can affect children’s dental, oral, or craniofacial health and development.
Cardiovascular Disease and Stroke
NHLBI and NIDCR Joint 75th Anniversary Symposium: The Science that Unites Us
Interested in learning more about oral-systemic health?
On May 16, 2024, NIDCR and the National Heart, Lung, and Blood Institute are co-hosting a virtual dual 75th anniversary symposium to showcase the science that unites the two institutes.
For more details, visit the event page.
Intrigued by their findings connecting oral disease to pregnancy complications, Drs. Offenbacher and Beck soon turned their attention to another set of conditions: cardiovascular disease and stroke. They’d recently learned of a report showing an unexpected link between cardiovascular disease and poor dental health, based on data that had been collected as part of the Centers for Disease Control and Prevention’s National Health and Nutrition Examination Survey (NHANES).
Drs. Offenbacher and Beck decided to follow up on this lead. They identified a link between periodontal disease in humans and certain precursors to heart disease and stroke, including thickening of the arteries and formation of a fatty substance called plaque in the arteries. Other physician-scientists found periodontal disease-related oral bacteria in heart valves removed during surgery.
In a study that evaluated the NHANES patients at a later point in time, researchers found that people who had periodontal disease early in the study were more likely to have a heart attack down the road. This study ultimately led to researchers suggesting that periodontal disease may be a heart disease risk factor.
Once other investigators established that inflammation increases the risk of heart disease, it became clearer that inflammation could be an important mechanism facilitating the relationship with periodontal disease.
“At the time, we weren’t having a lot of success convincing the medical community that inflammation could be a link between these conditions. They believed instead that heart disease and stroke were solely a problem with high blood lipids [fats],” said Dr. Beck. “Eventually, when the science caught up, the medical clinicians finally agreed that inflammation likely was a big problem across many chronic diseases and that several factors could contribute to cardiovascular disease simultaneously.”
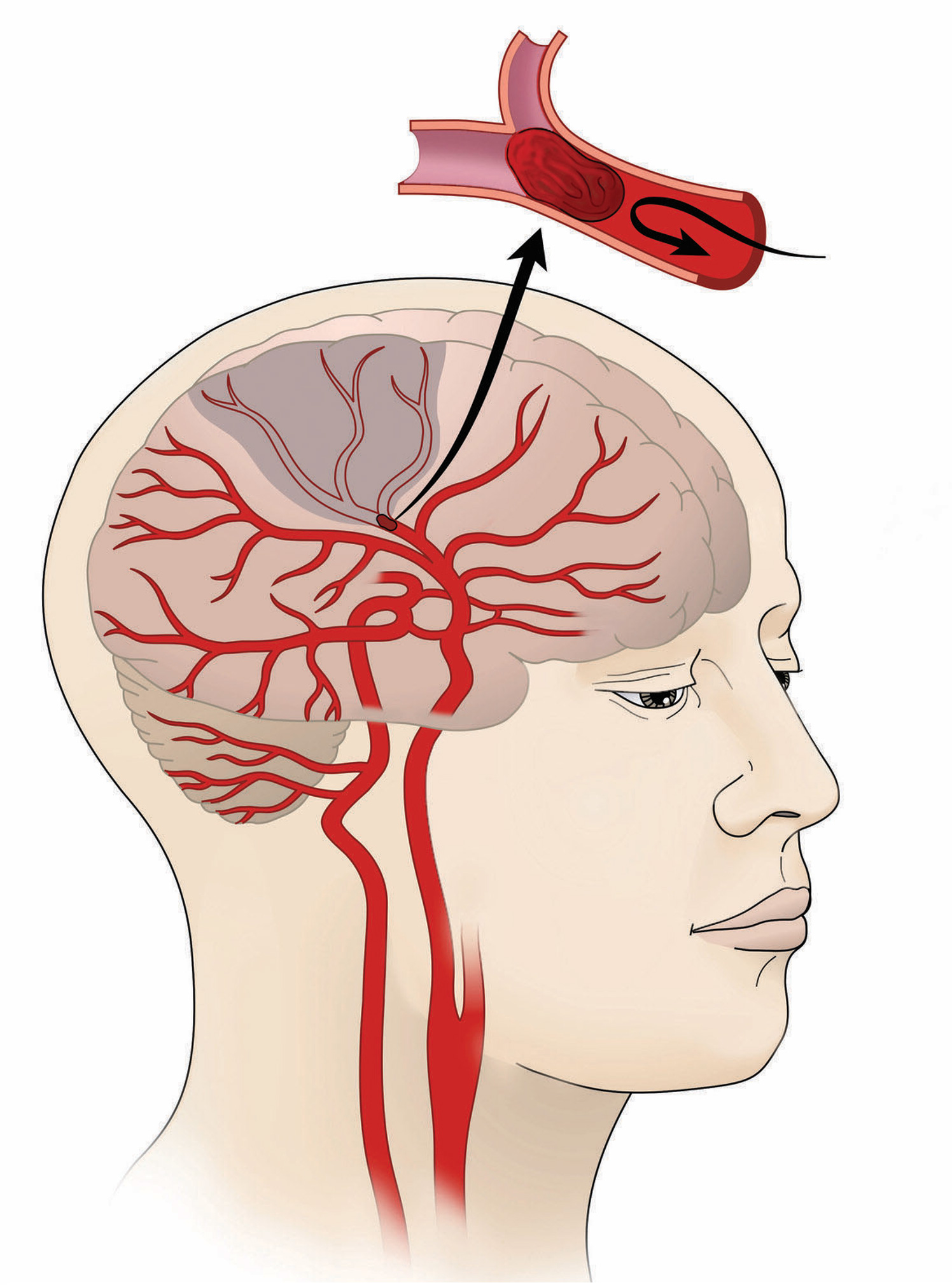
The prevailing theory nowadays for the relationship among cardiovascular disease, stroke, and periodontal disease proposes that harmful oral bacteria enter the bloodstream through tiny injuries in oral tissue caused by chewing or dental procedures. The immune system’s sentinels are thought to detect these circulating bacteria and ramp up inflammation to alert the rest of the immune system about the invaders. The responding immune cells then capture and kill many of these bacteria. But if the inflammation is prolonged (perhaps due to repeated episodes of bacteria entering the bloodstream), groups of immune cells may seed plaque formation on the inner walls of blood vessels. The remaining circulating bacteria may be trapped by immune cells in the plaque.
Over time, plaque can build up and cause blockages that lead to heart attack or stroke. Alternatively, pieces of this plaque can break off and form traveling blood clots. These clots can become lodged in an artery, causing a blockage and potentially a heart attack or stroke.
Dr. Beck and his colleagues have also looked for associations between tooth decay and stroke. Tooth decay, which affects about 90% of adults in the U.S., is more common than periodontal disease, which affects about 47% of U.S. adults over age 30.
In a paper published in Stroke in late 2023, Dr. Beck, stroke expert Souvik Sen, M.D., of the University of South Carolina, periodontal disease expert Cristiano Susin, D.D.S., Ph.D., M.S., of UNC, and their colleagues found that among more than 6,300 patients monitored over 21 years, cavities were associated with a 40% increase in risk of stroke and a 13% increase in risk of death by any cause. However, unlike periodontal disease, cavities weren’t linked to an increased risk of heart attacks.
Dr. Beck proposes that it’s harder to see associations between chronic systemic disease and tooth decay because tooth decay causes less pervasive inflammation than periodontal disease. People whose cavities are filled don’t experience severe inflammation unless they need a root canal. He said many studies have missed associations because they don’t include enough participants with severe enough disease for an effect to be apparent.
This same study found striking disparities between White and Black participants. Compared to White participants, Black participants with cavities were 150% more likely to have a stroke and almost 35% more likely to die of any cause.
“Oral diseases disproportionately affect the very same groups who experience disparities in chronic diseases such as diabetes, stroke, autoimmune illnesses, and heart disease,” said Dr. Webster-Cyriaque. “NIDCR embraces a whole health approach that encompasses all people and accounts for the intersections among oral health, systemic health, nutrition, inflammation, and the environment across the lifespan.”
Dr. Beck and others in the field recognize that studies showing an association between diseases only tell part of the story. To get at the causes of these connections, one must show that treating one disease can help alleviate the other.
In 2023, the same team published another study in Stroke that tested this relationship. The team assigned 280 patients who had periodontal disease and had experienced stroke to undergo traditional dental procedures (cleaning and dental plaque removal) or traditional treatment with the addition of more intensive procedures (use of local antibiotics on the gums and teeth, an electric toothbrush, and an electric air flosser). After about a year, both groups showed improvement in two risk factors: lower diastolic blood pressure (the bottom number that measures blood pressure when the heart is relaxed) and higher HDL, or “good” cholesterol. To ensure that these effects were due to the treatments and not to improvements in other risk factors for stroke, the researchers controlled for variables such as age, socioeconomic status, cholesterol and triglyceride levels, blood pressure, and more. However, the findings did not conclusively show that treatment of periodontal disease could prevent stroke recurrence.
According to Dr. Beck, this is the case with many cause-and-effect studies on periodontal disease. “Many of these studies implement one or two dental treatments, but these patients may still have a lot of sites in the mouth with periodontal disease at the end of the study,” said Dr. Beck. “The treatment itself isn’t sufficient to produce results demonstrating an advantage. Some people need surgeries or more intensive treatment to get them to better oral health that can’t be applied to all the other study participants. Other people may have so much inflammation in their bodies that it can’t be overcome by just treating the mouth.”
Dementia
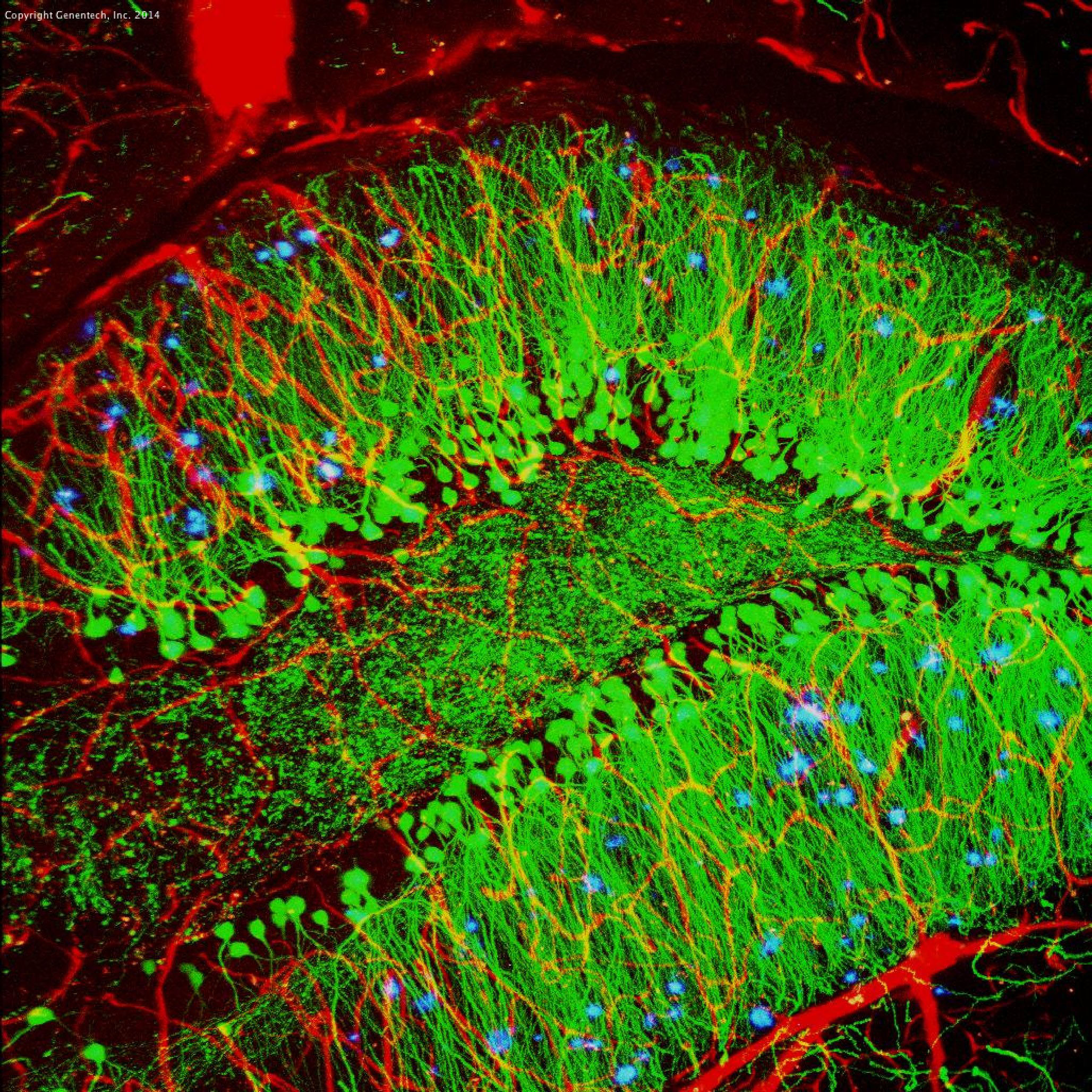
In certain cases, periodontal disease-related bacteria may colonize the body’s tissues, including the brain. Following the turn of this century, studies by NIDCR-funded researcher Panos N. Papapanou, D.D.S., Ph.D., of Columbia University and others demonstrated that people who had lost many or all of their teeth, had poor periodontal health, or had high antibody levels against certain periodontal bacteria were more likely to experience cognitive decline. Shortly thereafter, using brains from deceased people with Alzheimer’s disease, physician-scientists found periodontal bacteria (as well as gut bacteria) in the gunky clusters of amyloid protein — called plaques — that build up excessively in the brains of people with the disease.
Studies in mice showed that an infection in the mouth from periodontal disease-related bacteria led to an increase in amyloid protein in the brain and to cognitive decline. These findings spawned a newer theory that amyloid plaques may form as a way to fight infections or clear debris from the brain. Scientists are still trying to understand the exact role of amyloid protein in the body. How the mouth’s bacteria cross into the brain isn’t entirely known either, although some evidence suggests that they may travel through the body’s nervous system.
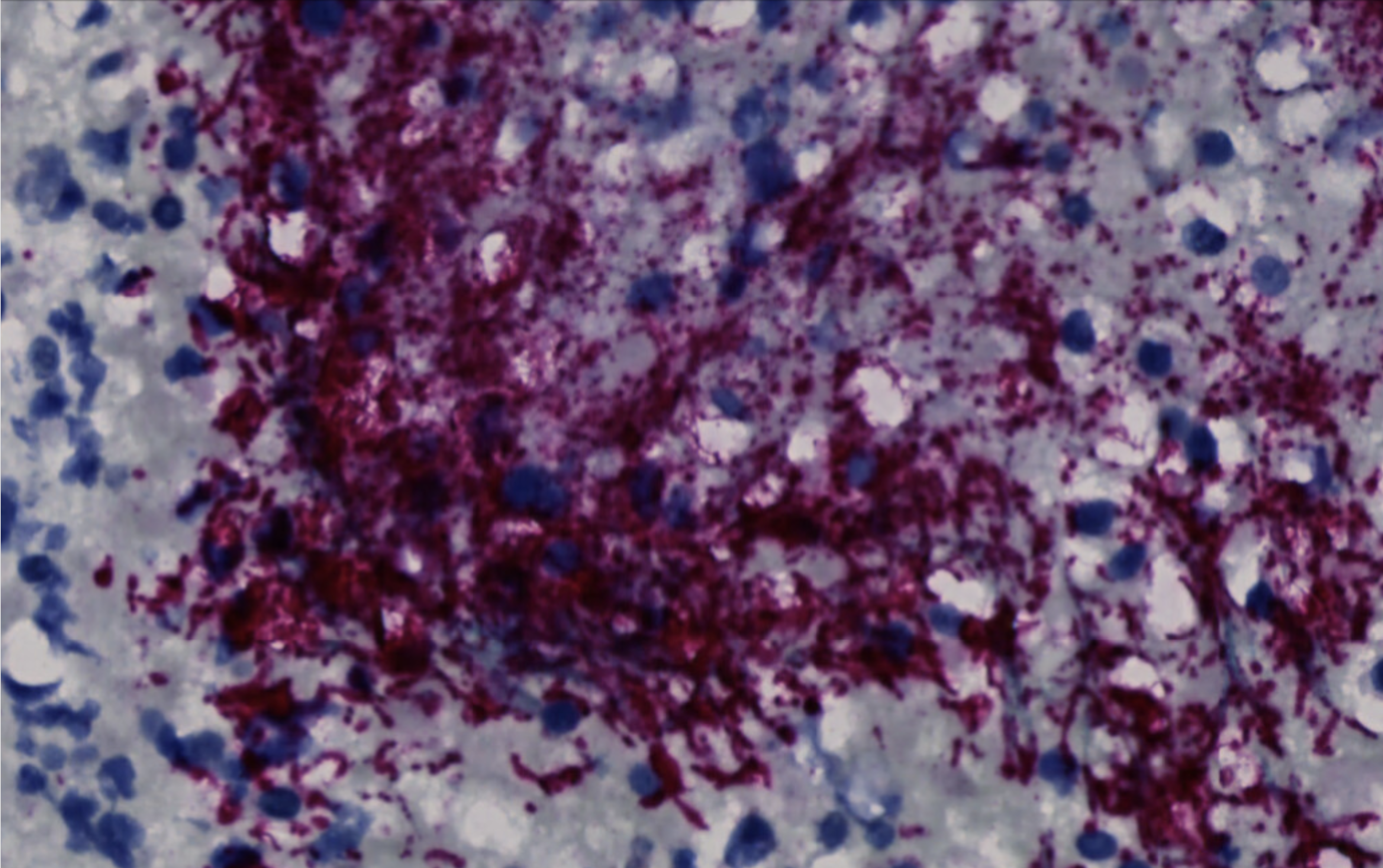
Cancer
Bacterial colonization may also contribute to certain cancers. Periodontal disease-related bacteria have been found in colon and rectal cancer and breast cancer tumors. Whether the tumors attract the bacteria, or the bacteria initiate tumor growth is still being worked out in the laboratory. However, research has demonstrated that the presence of these bacteria in colon and rectal tumors is tied to an increased likelihood of the cancer spreading, recurring, and worsening patient outcomes.
A study published on March 20, 2024, in Nature by NIDCR-funded investigator Christopher Johnston, Ph.D., and his team at the Fred Hutchinson Cancer Center, identified a niche strain of the periodontal disease-causing bacteria Fusobacterium nucleatum that appears in colon and rectal tumors. The niche strain was genetically distinct from the strain found in the mouths of people without cancer. When the scientists infected mice with the niche strain of F. nucleatum, the mice developed tumors anew in their intestines, suggesting that the bacteria could be capable of promoting cancer growth.
“We have pinpointed the exact bacterial lineage that is associated with colorectal cancer,” Dr. Johnston said. “That knowledge is critical for developing effective preventive and treatment methods.”
Now the researchers need to determine if the same strain can contribute to cancer in other human tissues, as well as whether other species of periodontal disease-related bacteria might also play a role in cancer growth and progression. Future studies can test if specifically targeting F. nucleatum in colorectal tumors can improve patient outcomes. Clinicians might also one day be able to screen for the niche strain to identify colorectal tumors that are more likely to be aggressive.
NIDCR’s Future in Systemic Disease
NIDCR continues to support work to tease apart the many factors involved in the oral-systemic connection. Prior to the pandemic, NIDCR began funding several research projects that focus on tailoring dental treatments for people with various inflammatory systemic diseases that could compromise their oral health. Then, to further boost its efforts in oral-systemic health, in 2021 NIDCR founded the Oral and Comprehensive Health Program, which supports extramural research that evaluates the interactions between oral health and general health throughout the lifespan.
Another avenue of ongoing research aims to dissect the molecular dance underlying the mutually inflammatory relationships among oral diseases and systemic conditions. For example, NIDCR currently funds studies in animals investigating the hypothesis that systemic inflammation from periodontal disease actually rewires the bone marrow stem cells that become immune cells in bone loss disorders and rheumatoid arthritis. These rewired immune cells, which are normally supposed to respond to infections, are instead erroneously “trained” to respond strongly to any little factor out of balance in the body by way of inflammation.
And scientists on an NIDCR-funded study at the University of Pittsburgh plan to use the extensive genomic data from NIH’s All of Us Research Program to search for genetic relationships between dental health and systemic diseases.
“NIDCR’s ongoing efforts to explore oral-systemic associations and identify underlying mechanisms continue to enhance research addressing whole person health and have the potential to transform patient care,” said Margaret M. Grišius, D.D.S., Director of NIDCR’s Oral and Comprehensive Health Research Program. “Understanding these relationships will open the doors for preventive measures and therapeutic interventions that could have an enormous impact on public health.”
Related Links:
References:
- Beck JD, Papapanou PN, Philips KH, Offenbacher S. Periodontal Medicine: 100 Years of Progress. J Dent Res. 2019 Sep;98(10):1053-1062. doi: 10.1177/0022034519846113.
- Löe H. Periodontal Disease: The sixth complication of diabetes mellitus. Diabetes Care 1993;16(1):329–334. doi: 10.2337/diacare.16.1.329.
- Hajishengallis G. Interconnection of periodontal disease and comorbidities: evidence, mechanisms, and implications. Periodontol 2000. 2022 Jun; 89(1): 9–18. Published online 2022 Mar 4. doi: 10.1111/prd.12430
- Jones JA, Moss K, Finlayson TL, Preisser JS, Weintraub JA. Edentulism Predicts Cognitive Decline in the US Health and Retirement Cohort Study. J Dent Res. 2023 Jul;102(8):863-870. doi: 10.1177/00220345231167805. Epub 2023 Jun 14.
- Dominy SS, Lynch C, Ermini F, Benedyk M, Marczyk A, Konradi A, et al. Porphyromonas gingivalis in Alzheimer's disease brains: Evidence for disease causation and treatment with small-molecule inhibitors. Sci Adv. 2019 Jan 23;5(1):eaau3333. doi: 10.1126/sciadv.aau3333. eCollection 2019 Jan.
- Zepeda-Rivera M, Minot SS, Bouzek H, Wu H, Blanco-Míguez A, Manghi P, et al. A distinct Fusobacterium nucleatum clade dominates the colorectal cancer niche. Nature (2024). doi: 10.1038/s41586-024-07182-w.
- Sen S, Logue L, Logue M, Otersen EAL, Mason E, Moss K, et al. Dental Caries, Race and Incident Ischemic Stroke, Coronary Heart Disease, and Death. Stroke. 2024 Jan;55(1):40-49. doi: 10.1161/STROKEAHA.123.042528. Epub 2023 Nov 29.
- Sen S, Curtis J, Hicklin D, Nichols C, Glover S, Merchant AT, et al. Periodontal Disease Treatment After Stroke or Transient Ischemic Attack: The PREMIERS Study, a Randomized Clinical Trial. Stroke. 2023 Sep;54(9):2214-2222. doi: 10.1161/STROKEAHA.122.042047. Epub 2023 Aug 7.
- Mattila KJ, Nieminen MS, Valtonen VV, Rasi VP, Kesäniemi YA, et al. Association between dental health and acute myocardial infarction. BMJ. 1989 Mar 25;298(6676):779-81. doi: 10.1136/bmj.298.6676.779.
- DeStefano F, Anda RF, Kahn HS, Williamson DF, Russell CM. Dental disease and risk of coronary heart disease and mortality. BMJ. 1993 Mar 13;306(6879):688-91. doi: 10.1136/bmj.306.6879.688.
Attention Editors
Reprint this article in your own publication or post to your website. NIDCR News articles are not copyrighted. Please acknowledge NIH's National Institute of Dental and Craniofacial Research as the source.
Subscribe for NIDCR Updates
Receive email updates about the latest advances in dental, oral, and craniofacial research.
October 2024